Menopause Brain Fog: The $26.6 Billion Crisis 75% of Women Face
Oct 11, 2025
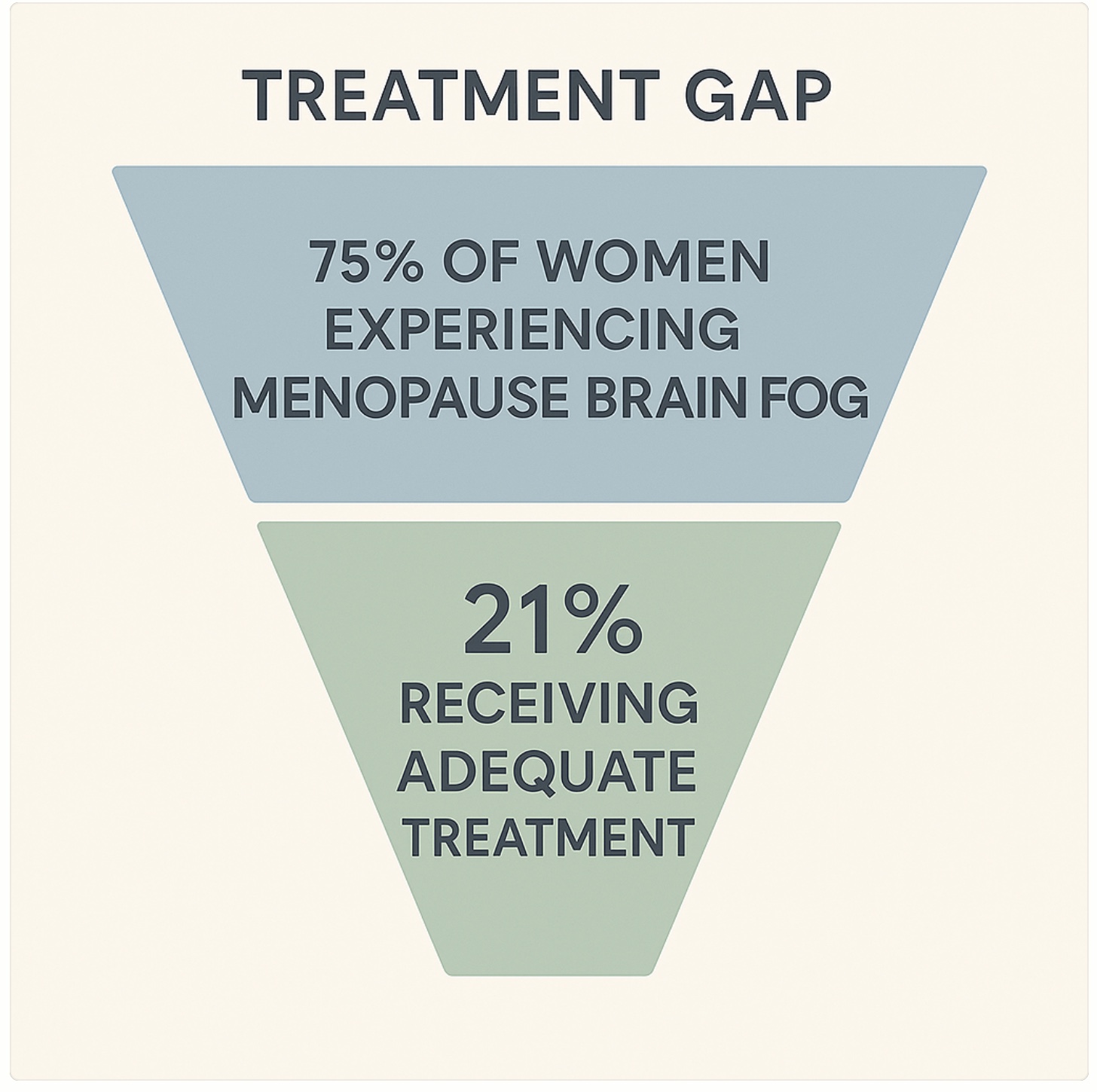
If you've been standing in your kitchen, staring at the coffee maker, completely forgetting what you came for, you're not alone. Brain fog affects 75% of women during perimenopause—yet only 21% get adequate care. Here's what research reveals about this costly, overlooked crisis.
Part 1 of 5: The Menopause Crisis America Ignores
If you've been standing in your kitchen, staring at the coffee maker, completely forgetting what you came there for... you're not alone. If you've sat in a meeting, watching your thoughts scatter like leaves in the wind while colleagues discuss projects you know you understand... you're not imagining it. And if you've wondered whether this mental fog that seems to roll in and out of your days has any real impact on your life... the answer might surprise you.
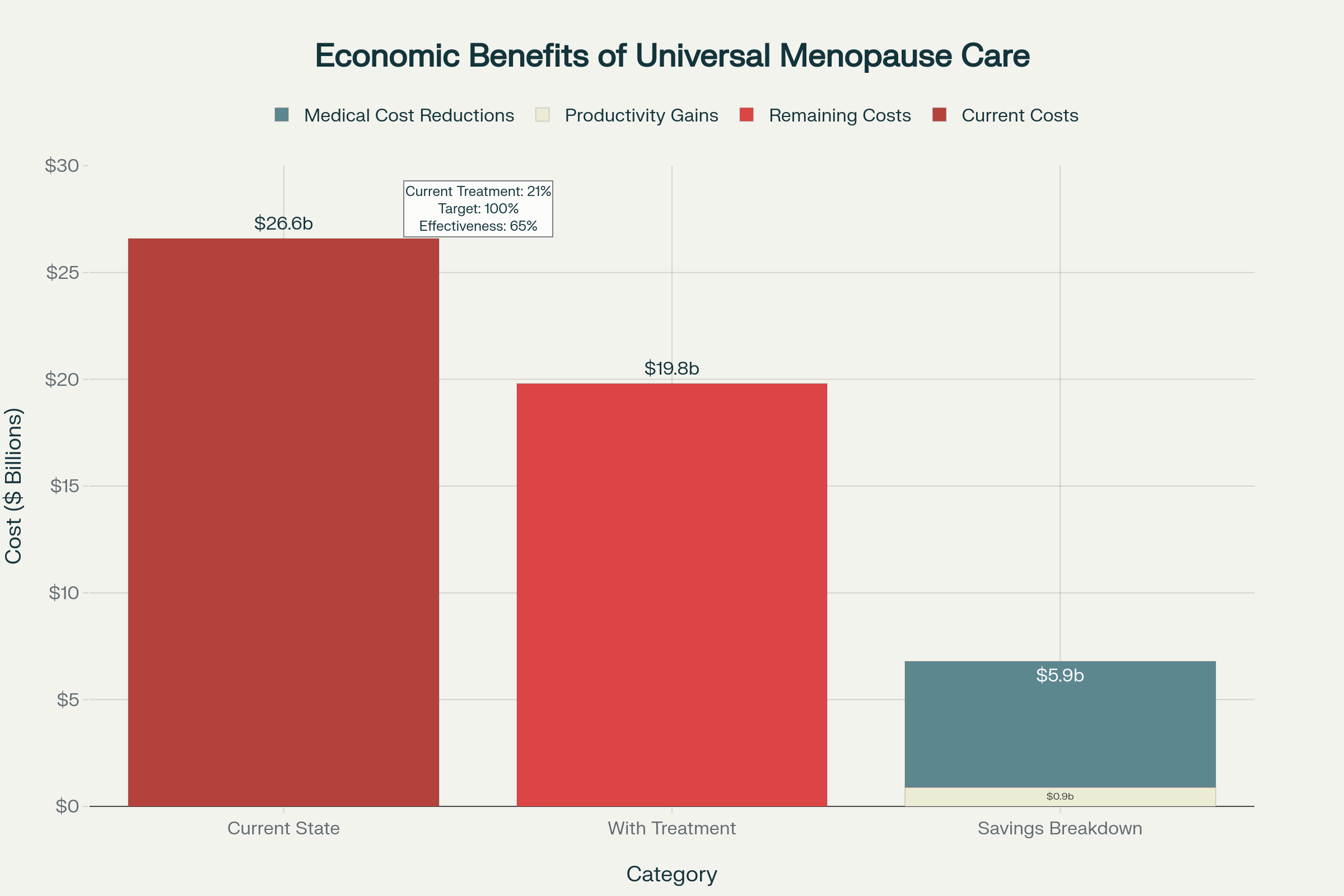
What you're experiencing has a name, a cause, and a $26.6 billion price tag that nobody talks about.
The Fog That Costs Billions: Understanding Menopause Brain Fog
Every day, 6,000 American women enter menopause. Every day, thousands more navigate the often turbulent waters of perimenopause, that transition period that can begin years before your periods actually stop. And for 75% of these women, brain fog becomes an unwelcome companion—that frustrating experience of mental cloudiness, forgetfulness, and difficulty concentrating that makes you feel like you're operating at half capacity.
But here's what nobody tells you: this isn't just a personal struggle you need to power through. This collective experience of millions of women has created an economic crisis that costs our country $26.6 billion annually. That's not a typo. Twenty-six point six billion dollars every single year.
To put that in perspective, that's more than the GDP of many countries. It's a crisis hiding in plain sight, affecting the most productive years of women's lives, and yet it remains largely invisible in healthcare policy and workplace conversations.
When "Just Getting Older" Isn't the Whole Story
Let's pause here for a moment. If you've been told this is just "normal aging" or that you should simply accept these changes as inevitable, you deserve to know the full picture. The brain fog you're experiencing during perimenopause and menopause isn't just about getting older—it's about hormones.
Research shows that perimenopause significantly impacts verbal learning, verbal memory, processing speed, attention, and working memory³. The hormonal changes during menopause, particularly declining estrogen levels, directly affect brain function in measurable ways. Estrogen influences neurotransmitter activity, enhances serotonin and dopamine function, and helps maintain blood flow to the brain—all crucial for memory, mood, and focus⁴.
This isn't weakness. This isn't failure. This is biology.
The Real Impact: From Personal Struggle to Economic Crisis
When 75% of women experience cognitive difficulties during their most productive career years, the economic impact extends far beyond individual struggles. The Mayo Clinic's landmark 2023 study revealed that menopause-related symptoms cost the U.S. economy $26.6 billion annually, comprising $1.8 billion in lost productivity and $24.8 billion in direct medical expenses.
Think about that for a moment. Nearly $2 billion in lost productivity because brilliant, capable women are struggling to think clearly through a treatable biological transition.
The workplace statistics tell a story that might feel achingly familiar:
- 90% of menopausal women report reduced productivity at work
- 75% experience brain fog and cognitive difficulties that directly impair job performance
- 45% take sick days specifically due to menopause symptoms
- 13% report adverse work outcomes including job changes, early retirement, or declining promotions
If you've found yourself declining opportunities, calling in sick more often, or questioning your professional capabilities, you're not falling behind—you're experiencing the effects of a health crisis that lacks adequate support.
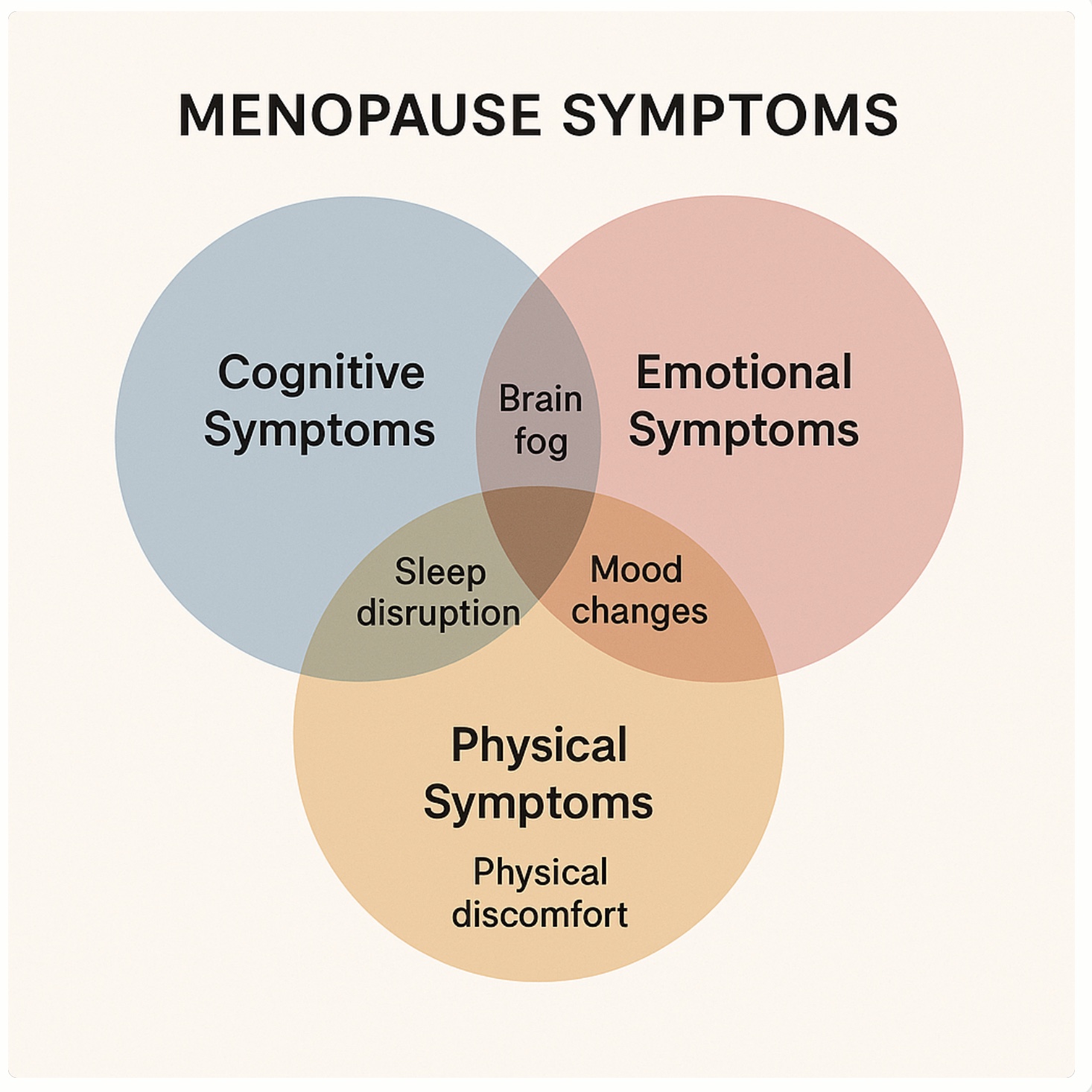
The Physical Symptoms That Compound the Struggle
Menopause brain fog doesn't exist in isolation. It's often accompanied by a constellation of symptoms that compound the cognitive challenges:
Sleep Disruption: 80% of women experience sleep disturbances during menopause, creating a cycle where poor sleep worsens cognitive function, which increases stress, which further disrupts sleep.
Mood Changes: 78% of women report mood changes including irritability, anxiety, and depression during the menopausal transition, making it harder to maintain focus and motivation at work and home.
Physical Discomfort: Hot flashes, joint pain, and energy fluctuations create additional stress on cognitive resources, leaving less mental energy available for complex thinking tasks.
Identity Confusion: Many women describe feeling like strangers in their own bodies and minds, leading to decreased confidence in their abilities and reluctance to take on challenging projects.
The Treatment Gap: Why Only 21% Get Help
Despite the significant impact on quality of life and economic productivity, only 21% of women experiencing menopause symptoms receive adequate treatment⁵. This massive treatment gap exists for several interconnected reasons:
Healthcare Provider Knowledge Gaps: Many healthcare providers lack comprehensive training in menopause management, with only 30% of OB-GYN program directors reporting adequate menopause curricula in their training programs.
Stigma and Silence: Cultural taboos around discussing menopause mean many women suffer in silence, assuming their struggles are just part of "getting older" rather than symptoms of a treatable medical condition.
Conflicting Information: Confusing and sometimes contradictory information about hormone therapy safety has created fear among both patients and providers, limiting treatment discussions.
Time Constraints: Brief medical appointments often don't allow for comprehensive discussion of complex menopause symptoms and treatment options.
The Power of Understanding: Your First Small Step
Here's where the Power of Little philosophy becomes especially important. You don't need to fix everything at once. You don't need to become an expert in hormone therapy or menopause research overnight. You don't need to completely overhaul your life.
Sometimes the most powerful step is simply understanding that what you're experiencing is real, valid, and shared by millions of women. Sometimes it's recognizing that your struggles have been measured, studied, and validated by researchers who found them significant enough to quantify in billions of dollars.
This understanding can be the gentle beginning of advocating for yourself—whether that's having a different conversation with your healthcare provider, researching treatment options at your own pace, or simply giving yourself permission to acknowledge that this transition deserves attention and support.
Small Shifts That Can Make a Big Difference
While you're processing this information and considering your next steps, here are some gentle approaches that align with the Power of Little philosophy:
Document Your Experience: Keep a simple symptom journal noting when brain fog is worst, what might trigger it, and what helps. This information becomes valuable when discussing treatment options with healthcare providers.
Educate Yourself Gradually: You don't need to research everything at once. Start with one reliable source (like the North American Menopause Society website) and learn at your own pace.
Connect with Others: Whether it's an online support group, a trusted friend, or a healthcare provider, breaking the isolation around these experiences can be powerfully healing.
Practice Self-Compassion: On days when your thinking feels unclear, remind yourself that this is a temporary biological transition, not a reflection of your intelligence or worth.
Explore Gentle Support: Simple interventions like regular sleep schedules, stress reduction techniques, and appropriate nutritional support can sometimes provide meaningful relief while you consider other options.
A Moment of Hope: July 17th Matters
In five days, something important is happening that could change the landscape of menopause care in America. On July 17th, an expert panel at the FDA will discuss removing the black box warning on vaginal estrogen—a change that could dramatically improve access to one form of treatment that many women find life-changing.
This panel represents more than a policy discussion; it represents hope for the millions of women who have been struggling in silence, wondering if there's something better than "just dealing with it."
The black box warning has created unnecessary fear around a treatment that research shows to be both safe and effective for many women experiencing vaginal dryness, painful intercourse, and urinary symptoms. Removing this warning could increase access to care and reduce the stigma that prevents both healthcare providers and patients from considering appropriate treatments.
Your Experience Matters: The Ripple Effect of Recognition
When you begin to understand that your brain fog, your workplace struggles, your sense of moving through mental molasses isn't personal failure but part of a documented health crisis affecting millions, something shifts. You move from feeling isolated and defective to recognizing yourself as part of a larger story that deserves attention, resources, and respect.
This shift in perspective can be the beginning of everything—from seeking appropriate healthcare to advocating for workplace policies that support women through this transition, from connecting with other women navigating similar challenges to simply treating yourself with the compassion you'd offer a friend experiencing the same struggles.
What Comes Next in This Series
July 14th: Why 75% of women are struggling in silence at work—and how untreated menopause symptoms are creating a workplace productivity crisis that affects entire organizations.
July 15th:The relationship toll nobody talks about—how menopause symptoms are contributing to divorce rates and family stress, and why love alone isn't enough when symptoms go untreated.
July 16th: The science of reclaiming your mental clarity—evidence-based treatment options that can restore cognitive function and help you feel like yourself again.
July 17th: How you can be part of the change—specific ways to support policy changes that could improve menopause care for millions of women.
Each piece will include resources, gentle next steps, and the kind of evidence-based hope that comes from understanding that your experience matters—not just to you, but to the millions of women walking this path alongside you.
The Beginning of Change
If you've read this far, you've already taken a small but meaningful step. You've chosen to spend time learning about something that affects your daily life. You've decided that your experience deserves understanding rather than dismissal.
That's not a small thing. That's actually the beginning of everything.
Whether you're in the thick of perimenopause, navigating menopause, or supporting someone who is, remember this: the fog you're experiencing doesn't define your capability, your intelligence, or your worth. It's a temporary weather pattern in the climate of your life, and like all weather, it can change.
Sometimes it changes with time. Sometimes it changes with treatment. Sometimes it changes with understanding, support, and small steps toward advocating for the care you deserve.
The most important thing to remember is that you're not alone in this fog. Millions of women are navigating the same cloudy territory, and together, we can work toward a future where this transition includes the support, understanding, and treatment that every woman deserves.
Tomorrow, we'll talk about what's happening in workplaces across America, and why your career struggles during this transition aren't about your professional abilities—they're about a healthcare gap that affects millions.
Until then, be gentle with yourself. You're navigating something significant, and you're doing it with more strength than you probably realize.
Want to be part of the change?
Learn more about the July 17th FDA panel and how to add your voice at Unboxing Menopause
Your experience matters, and your voice can help create the changes that millions of women desperately need.
*This post is part of a 5-part series exploring the hidden economic and social costs of inadequate menopause care in America. Each day through July 16th, we'll examine different aspects of this crisis and the hope for transformation that July 17th represents.
References
- Mayo Clinic. (2023). Menopause in the workplace: Challenges, impact, and next steps. Mayo Clinic Proceedings
- AARP Public Policy Institute. (2024). Menopause in the workplace: Impact on productivity and career advancement
- Harvard Health Publishing. (2016). Changes in memory tied to menopausal status. Harvard Gazette
- Jean Hailes for Women's Health. (2024). The fog of menopause: Understanding cognitive changes
- AARP Research. (2024). Menopause women untreated: Healthcare gaps and accessibility issues
Download the complete research guide here: Full Research Guide
Weekly Gentle Support for Your Midlife Journey
Gentle prompts, science-backed tips, and stories of tiny wins — delivered every Friday.
By subscribing, you agree to receive ongoing updates